SVH COVID-19 Community Update
Efforts to slow the community transition rate of the coronavirus here in Sonoma Valley are working, as demonstrated by a decrease in the numbers of new cases week over week in the Bay Area as well as a decrease in the number of individuals hospitalized with COVID-19. These are all good signs we are headed in the right direction, and there is no need for community members to delay using the hospital for essential health services.
All hospital services, including Outpatient Diagnostic Testing, Rehabilitation, Wound Care, Occupational Health, and Infusions are operational and scheduling patient visits. We are also now scheduling some non-emergent surgeries, which will resume next week.
Our Emergency Department remains open 24/7 as always, and our COVID-19 hotline and drive-through testing remains open.
We continue to take precautions with patients within the Hospital, with rigorous sanitizing protocols in place and physical distancing practiced in waiting areas. We ask patients to bring a facial covering for visits if you have one. If not, we will provide one.
We remain committed to keeping our community informed on the COVID-19 crisis, but as we are now turning our attention to recovery, our updates will be less frequent, although we will continue to share important information as it becomes available.
COVID-19 Q&A
We have received many questions from our community about COVID-19, its effects, tests and potential treatments. We recently received information from UCSF Health that answers many of these questions, and we have included them at the end of this update.
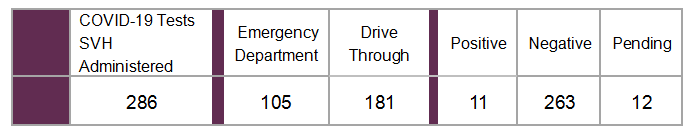
Testing By the Numbers:
Through April 30, 2020
COVID-19 Screening Hotline & Testing
Calls made to the hospital’s COVID-19 Screening Hotline, 707.935.5440, are answered by a Registered Nurse between 8:00 am and 4:00 pm, seven days a week. Calls made before 8:00 am and after 4:00 pm receive a prerecorded message asking the caller to either call back the next day or, if immediate attention is needed, to call 911 or go to the nearest Emergency Department.
During the evaluation, if it is determined that testing is indicated, patients are given an appointment for the drive-through screening site where testing occurs. The appointment-only testing is located in the north entrance parking area of the hospital (just west of Third Street West off of Andrieux Street).
Information Is Available On Our Website
We encourage you to take care of yourself and your family members by following government guidelines, including maintaining social distancing and practicing good hand hygiene. Information on recommended practices is available on our website. As we navigate through this situation together, we will provide regular updates at our website and through our email and social media communications.
COVID-19 Q&A (Prepared By UCSF Health)
What tests are available for COVID-19?
There are two main types of tests for COVID-19. Reverse transcriptase polymerase chain reaction (RT-PCR) directly detects active viral infection. Serology tests detect immune response (antibodies) to infection, which typically takes at least two to three weeks to develop.
What is a serology or antibody test?
Serology blood tests are designed to identify who has previously been infected with COVID-19. They look for an immune response to the coronavirus in the form of a specific protein material, or antibodies, in your blood.
If a person has antibodies to the coronavirus, does that mean they are immune to getting it again?
We currently don’t know whether antibodies to the SARS-CoV-2 virus offers immunity against future infections and if so, for how long. Several other coronaviruses have limited or short-term immunity after an infection, but it is too early in this epidemic to understand whether or how antibodies will protect people who have had COVID-19. We will need more studies to determine if the presence of antibodies means a person won’t get re-infected. Until those studies are done, decisions about returning individuals to work or school should not be based on antibody test results.
How soon after infection does someone start producing antibodies?
Antibodies can appear approximately one week after infection and typically peak four to six weeks after symptoms begin. Most people will develop antibodies within two to three weeks after infection. Some patients, particularly those with immunocompromising conditions, may not produce a detectible antibody response.
How long after infection do antibodies remain in the body?
The length of time that antibodies remain in the body after infection is not well known for SARS-CoV-2. For most viruses, antibodies remain detectable for months or sometimes even years after infection.
What is hydroxychloroquine?
Hydroxychloroquine is in a class of drugs that are primarily used to treat malaria, but also are used to treat discoid or systemic lupus erythematosus and rheumatoid arthritis in patients whose symptoms have not improved with other treatments.
Is hydroxychloroquine effective in treating patients with COVID-19?
We currently don’t know. There have been a few small studies that have not answered key questions and have shown evidence of harm by using chloroquine and hydroxychloroquine in patients with COVID-19. This demonstrates the importance of not using these drugs off-label and instead testing them in clinical trial settings where we can monitor patients.
What is remdesivir?
Remdesivir is an investigational antiviral compound undergoing clinical trials in China, the United States, and the United Kingdom as a potential treatment for COVID-19, including at UCSF Health. It is not yet licensed or approved anywhere globally.
Is remdesivir effective in treating patients with COVID-19?
Published studies have not yet demonstrated the benefit of the use of remdesivir. However, a recent report from the National Institutes of Allergy and Infectious Diseases has reported improved clinical outcomes in a large randomized control trial in the United States in patients taking remdesivir compared to those taking placebo. Publication of this study through a process of peer review is pending as are several other studies using remdesivir.
Where do we stand in the development of a COVID-19 vaccine?
In response to the global COVID-19 pandemic, the global vaccine research and development effort has moved at an unprecedented speed. Based on the scale and speed at which vaccine development is proceeding, there is an indication that a vaccine could be available at some time in 2021 under emergency use protocols.