SVH administration has recommended to the Sonoma Valley Health Care District Board closure of the Hospital’s Obstetrics service in 2014. Healthy births would be handled elsewhere and only women with obstetrical emergencies would be treated by the Hospital in its Emergency Department.
The reason for this is that SVH does not have enough births to justify the high costs of maintaining the service, and the number of births continues to decline. This has been a difficult decision for the Hospital to arrive at, but a necessary one in the view of Hospital administration.
Following is a copy of the entire report presented to the Board on January 9, 2014, which provides the rationale for this recommendation.
|
Meeting Date: January 9, 2014 Prepared by: Kelly Mather and SVH Administrative Team Agenda Item Title: Financial Viability Plan for 2014 Introduction Sonoma Valley Hospital must continually and conscientiously address the challenges of a rapidly changing health care environment in order to create a financially stronger and more sustainable Hospital. The cost of running a full-service inpatient, acute care hospital continues to increase and SVH has responded by reducing expenses significantly over the past four years. Due to lower than expected volumes and a changing payer mix forecast for 2014, SVH is again reviewing and reducing costs of hospital operations. One component of the approach is a departmental review under my direction and responsibility as CEO. In December, 2013, each hospital department was reviewed and leaders were asked to submit an action plan to reduce expenses in their departments. We have begun implementing the majority of these changes and the result will reduce expenses. These include reducing annual expenses in the following areas: Surgery, Med/Surg, Ancillary Services, Environmental Services, Dietary, Physicians and Information Technology. Reductions in these areas do not result in layoffs. In the past year, after months of careful assessment of our future, we adopted a new strategic plan. This plan determined that SVH has 11 major service units. One unit, Emergency, has a very high community demand and it has been agreed that providing Emergency Care is our first priority. This unit is very costly for a small hospital and it is supported by the annual parcel tax. Five of the eleven of our service units currently have a positive margin. They are: Surgery, Home Care, Skilled Nursing, Outpatient Services and Rehabilitation. As we have previously discussed, there are 4 service units that are close to break even, but provide a return on the investment by providing important foundational services. They are: Inpatient (ICU/Med/Surg), Occupational Health, Wellness and Special Procedures. The last service unit, Obstetrics, has had questionable viability for many years. Obstetrics currently loses approximately $86,000 per month and has very low demand from our community. Due to the necessity for future financial health and after exhausting all possible avenues to increase the volumes to make this service viable, we recommend Obstetrics be closed. This component of the plan requires board action. Volume Analysis Using OSHPD obstetrics data for SVH’s combined service area, the volumes are as follows:
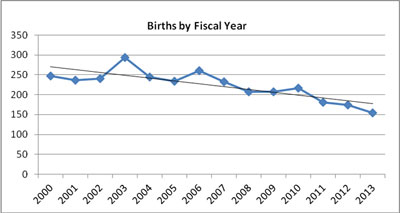
SVH’s OB Department has seen a decline in annual births from calendar year 2000. From 2000 to 2006 the average number of admissions to OB was 252 annually (21 patients/month) or 0.7 patients per day. During the period 2007-2012, the average number of admissions to OB was 203 annually (17 patients/month) or 0.6 patients per day. For 2013 the OB Department has seen 154 patients or an average of 0.4 patients per day. Currently, the department sees about 12 patients a month. Some have asked, “why can’t we market the program and save it?” For over 5 years, SVH attempted to recruit a female OB to increase the volumes. Each candidate declined due to the fact that there is simply not enough demand (or births) in the Sonoma Valley area for a sustainable practice. Today there is one OB physician to support the Obstetrics program and it is very unlikely that his volume would increase above 20 patients. Kaiser Permanente has 20% of the market share, which is unlikely to change much. Finally, many patients choose female or out of area Ob/Gyn’s which accounts for even lower volumes. Marketing is not an answer when the market only has a potential of attracting 22 prenatal mothers per month and they would all have to choose our hospital. Regulatory Requirements: SVH has maintained a quality OB program, but at a very high cost. The Hospital’s ability to adjust its services to reflect decreasing demand is restricted by existing regulations. Title 22 regulations for the State of California require two OB-competent RNs to staff the department when patients are present. Each RN may take care of one to two moms in active labor or four moms and babes in the post-partum environment. This requirement is 24/7 and even when the census in the department is zero, which is at least half of the time, one RN must be present at all times to accept a patient. The nurse cannot be assigned on another nursing unit as she must be available to accept an arriving mom. The second RN is placed on standby and, if called in, is paid time-and-a-half pay. Cost and Un-productivity due to Regulations: For purposes of this discussion, we will assume the department is staffed with two RNs for 15 days/month (0.5 patients/day) and staffed with one RN in-house and one RN on standby the remaining 15 days/month. Our SVH RNs earn an average of $58/hour. Conservatively measured, 15 days a month two RNs are needed each shift and the annual salary and benefit cost to keep this service unit open for 13 patients a month is over $1.43 million per year. Each OB RN must also retain competency in Neonatal Resuscitation Protocol (NRP), Advanced Fetal Heart Monitoring (AFHM) and Advanced Cardiac Life Support (ACLS). These competencies are renewed every other year. Additionally, there is the California Breast Feeding Initiative and the Beta Health Quest for Zero initiative which add to further education (and cost) for the OB RN. Competency training and maintaining best practices for all of the OB RN’s is very costly. Further, an Obstetrics Department with an average monthly census of 13 has a difficult time attracting and retaining nurses. Nurses understandably want to be busy and yet, at least 15 days a month, nurses sit in the SVH OB Department waiting for moms to show up. This shows up in the turnover rate for our OB Department, which is 36% compared to less than 8% for the rest of the hospital. Because of this, the department often is forced to train OB RNs, which is costly. Depending on the level of experience, training an OB RN can take two weeks to 12 months. The regulatory requirements for maintaining an Obstetrics department in an acute care hospital do not allow for flexibility or reducing nursing labor expenses. Financial Analysis: For the past few years, the hospital has elected to show the OB program as financially supported by the Medicare Disproportionate Share (DSH) payment. Due to the continued changes and reductions in reimbursement, we do not think this is a valid way to analyze the department going forward. Up until December, the DSH payment was being reduced by 75% in compliance with the Accountable Care Act. We anticipate it will be reinstated and will be in effect until October, 2015. Based on communications from the California Hospital Association, the estimated annual payment under DSH will be $522,600. Even with the DSH payment, Obstetrics department still does not have a positive financial contribution. We need approximately 23 births per month to break even. The following is a summary of the OB Department financials:
The Medical Executive Committee and the Chief Medical Officer support closure of the department based only on current financial impact and lack of patient demand. The physicians clearly state that SVH does not have any quality concerns, but are aware of Obstetrics not having enough patients for sustainability. The physicians are also aware that many hospitals, especially small ones with local Ob options, do not offer Obstetrics due to the regulations and costs. The discussion of the possible closure of this service was discussed at length by the Medical Executive Committee. Two of the physicians who will be affected the most by this decision shared their concerns about closure. While the physician leadership does not want to close a service that is important to their colleagues, the Medical Executive Committee said they believe that the hospital’s future financial viability is of more importance than keeping a service with very low patient demand and voted to support this recommendation. Employees: Currently there are fourteen (14) staff members designated specifically to the OB unit. Should the decision be made to close the OB unit we would offer a retention bonus and the usual severance. The SVH staff members are aware of this recommendation and the response has generally been one of understanding. There are differing opinions about what we could have done to “save OB” but almost every suggestion has been tried. Closure Plans: The move to close the service would take between three and four months, based on what other hospitals have experienced. This allows time to communicate the decision to the community and allow prenatal women the time to find alternate delivery options, which are currently available within the area. There are 4 local hospitals with Obstetrics programs, a birth center nearby and many patients are now delivering at home. New policies will be developed regarding protocols when women in active labor or women with obstetrical emergencies arrive in our emergency room. Nurses and physicians both will need to be trained in neonatal resuscitation, and nurses would attend deliveries at a high-volume hospital to gain additional training. A new operational relationship between our obstetrical providers and pediatricians would be developed regarding call coverage for the event of an obstetrical or neonatal emergency. Transfer arrangements will need to be made with the hospitals that offer nearby obstetrical coverage. A discussion with our local Fire Med regarding a transfer policy and the requirements for patients that are in labor would be undertaken. In addition, if the service is closed, we will need to take plan this to the Sonoma County Board of Supervisors. Communications: The community has been informed that this recommendation is being presented in early 2014. We have spoken candidly with many stakeholders and laid the facts out for input and discussion with organizations and community members, such as the Health Center, throughout the month of December. Everyone thinks it is an unfortunate situation, but most seem to understand that the hospital must provide services that are in demand and cannot sustain this program to the detriment of the vital services that are highly utilized. This has been part of an ongoing conversation the Hospital is having with the community about our priorities within the financial constraints we face in a changing health care landscape. The education of the community about the hard choices that must be made to maintain a hospital in a small town has been going on for years and will continue as we adapt to the rapidly changing health care environment. Consequences of Negative Action/Alternative Actions Alternatives to closing the Hospital’s Obstetrics Department include:
Financial Impact The hospital loses $86,300 per month due to the Obstetrics program. |